Prevalence and Socio-Economic Impact of Gastro-Intestinal Illness and Leaky Gut.
Abdominal pain and fatigue are two of the top ten reasons individuals seek the attention of a physician . Fatigue, while not in and of itself necessarily associated with gastro-intestinal (GI) dysfunction, is one of the many symptoms associated with it. There are a variety of causes of gastro-intestinal illness including: parasites, Crohn’s Disease, Ulcerative Colitis, and Irritable Bowel Disease (IBS), and leaky gut.
The extent of the impact of GI dysfunction in our society is far-reaching. A 2014 compilation of US disease statistics undertaken by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) indicated that in 1998, Irritable Bowel Syndrome (IBS), afflicted 15.3 million people and a more recent estimate indicates that Crohn’s and Ulcerative Colitis may currently afflict approximately 1 to 1.5 million people, in the United States (US) alone . These former numbers are undoubtedly understated given population growth since the studies were completed.
IBS also puts a heavy economic burden on the health care system. Estimates have shown that more than $10 billion in direct costs and $20 billion in indirect costs can be attributable to IBS each year in the US Results from another 2008 study estimate that the annual direct costs of Crohn’s and Ulcerative Colitis in the United States add an additional $3.6 billion and $2.7 billion to overall US health care costs .
Digestion, Inflammation and Disease
Digestion, or rather, the body’s inability to digest food, is what irritates the GI System leading to a myriad of symptoms such as: gas, bloating, belching, flatulence, abdominal pain, diarrhea and/or constipation. The impact of the body’s inability to absorb nutrients from digestion, food allergies/sensitivities, bacterial and/or yeast overgrowth and/or “leaky gut”, in turn, may lead to other systemic symptoms such acne, anxiety, depression, autism, neurological disorders, autoimmune diseases as well as some forms of cancer.
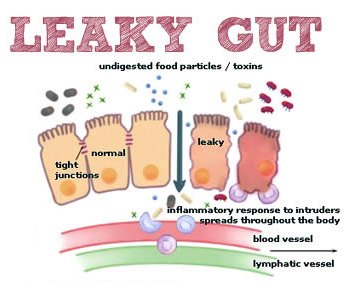
Leaky Gut, medically termed “intestinal permeability” results from an unhealthy intestinal lining. Gaps are created between cells in the intestinal wall, allowing undigested food and other toxins present in the food to “leak” into the blood stream and trigger an immune response. In contrast, a healthy gut processes foods in a systematically well-calculated process allowing for proper absorption, transportation, assimilation and excretion of nutrients and waste products respectively. The following diagram provides a simplistic overview of leaky gut.
There are a number of possible causes of leaky gut but I would like to focus on the role of one of the first organs in the digestion process (after mastication), the stomach, in leaky gut and other gastro-intestinal symptoms and ailments.
The Stomach and the Gastric Acid Balance
Healthy digestion requires that the stomach secretes Hydrochloric Acid (HCI) and maintains acidity at a specific level. The major function of HCI is to sterilize pathogens in food in order to reduce chances of infection and disease. It does this by inhibiting the growth of these pathogens (e.g., viruses, bacteria, yeast and fungus), by creating a hostile environment inhibiting the survival and replication of these microorganisms.
From a practitioner standpoint, I am convinced that the digestive processes of the stomach is the most important component of the entire system. At a minimum, the activities which take place in the stomach are critical precursors to all the other digestive processes which follow.
In addition to sterilizing food pathogens and nutrient conversion, HCI stimulates very important hormonal functions which signal the small intestine, the pancreas and the liver/gallbladder to produce enzymes and other secretions to help us properly digest food and absorb the nutrients contained within food to keep our body healthy and functioning at its optimal level.
To be more specific, HCI, during the first stage of protein digestion, unfolds and breaks down proteins into its amino acid precursors, for use by the body, by activating the conversion of inactive pepsinogen, an enzyme secreted by the chief cells of the stomach, to the active pepsin, our very powerful proteolytic enzyme which further breaks down protein to its amino acid constituents.
In the case of low HCL secretions, sterilization of food stuffs is inhibited, setting the stage for opportunistic (non-beneficial) bacteria to infiltrate the intestinal tract and food nutrients are not converted. In low stomach acid (hypochlorhydria) the proteins we consume become undigested allergens leading to in many instances, full-blown food allergies, sensitivities, and the development of other GI disorders such as dysbiosis (an overgrowth of yeast, bacteria and/or pathogens) and small intestinal bacterial overgrowth (SIBO), which is mainly due to the presence of bacteria in the upper gastrointestinal tract that is normally found in the colon.
Under healthy conditions, the stomach has a very low pH (high acidity) for approximately twenty minutes before the pH begins to rise (lower acidity). A pH of between 4.0 and 4.5 is the required threshold for triggering the pyloric valve (which controls the opening between the stomach and the small intestine) to open and allow the next stage digestion in the small intestine to proceed. The small intestine is where approximately 90% of the minerals and other nutrients from our food are absorbed into the bloodstream.
Low stomach acid (hypochlorhydria), inhibits the body’s ability to absorb many nutrients such as Vitamins A, D, E, K and B12 which is a leading cause of malnutrition. Many factors lower HCI secretion such as: age, antibiotics, proton pump inhibitors (PPI’s), over-use of antacids and alcohol, anti-mucus medications, antihistamines and H. Pylori and Campylobacter infections. Hypochlorhydria also reduces GI motility, resulting in constipation which further leads to putrefaction of undigested protein, rancidity of fats and fermentation of carbohydrates, and in turn creates the perfect environment for opportunistic (bad) bacteria to flourish. When HCL production ceases (achlorhydria), foods are no longer sterilized and proteins are not converted to amino acids. The body in essence “starves” – malnutrition and anemia set in.
In contrast, high stomach acid (with a low pH) or “hyperchlorhydria” can lengthen the time the digested food remains in the stomach before proceeding to the small intestine, potentially leading to more serious issues such as peptic ulcers, gastro esophageal reflux (GERD), hiatal hernias or in severe cases, gastric cancer. High stomach acids have also been linked to reduced secretions of pancreatic enzymes into the small intestine. Pancreatic enzymes are critical in the process of fat, protein and carbohydrate digestion. Insufficient enzymes can increase the probability of infections and diarrhea.
A confounding factor is that the symptoms associated with both low and high stomach acid are very similar which is why it is very important to ensure that the appropriate diagnostic testing is undertaken. There are some simple home tests that may help indicate where on the acid spectrum one lies, however, in order to determine actual HCL levels, more conclusive testing from a Heidelberg Radio-telemetric Device or Gastro-Testing may be warranted. Take a look also how genetics can play a role.
In summary, healthy levels of hydrochloric acid secretion is the first and most important step in achieving and maintaining optimal health. Testing and monitoring of HCL should be a priority when searching for the root cause of gastro-intestinal illness or discomfort, and should also comprise part of the analytical protocol used to assess and treat other auto-immune and inflammatory disease.


Great article highlighting the importance of HCl in the stomach. Now, exactly where and how does one get the testing to determine the current level of acid and what needs to be done to get an optimal level?
Thank you Jack!
Since I was a kid I have been suffering with Gas, ibs ,acid reflux .Now I am taking Atrantil that give big relief with gas bloating, right now acid reflux. I was diagnostic with Celiac disease with inflammation in Upper Gi.What I need to know the best supplement to relieve it
.
Hi Lucner
You need to eliminate the foods that are causing inflammation, use natural substances that mimic your body’s natural physiological processes such as a sodium/potassium bicarbonate product as well as digestive enzymes, and heal the gut with proper nutrients.